Functional Movement is Negatively Associated with Weight Status and Positively Associated with Physical Activity in British Primary School Children
Posted by Kyle Barrow
Thinking back, my first focus on movement occurred during farm work and playing in the woods. Watching the way that animals on the farm and animals in nature moved, and how different it was the way that I moved. When I got into athletics, I started comparing myself to my teammates and my competition as we performed movements seeking the same outcome and realized there was a difference there as well.
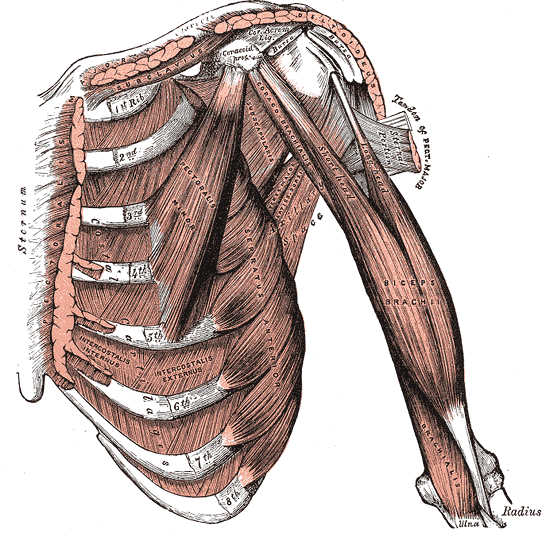
My interest in movement carried me into an undergrad degree in Exercise Science and Sports Medicine. That was my first exposure to the concept of Kinesiology: how every muscle in the body had been mapped, how its attachment points were called origin and insertion and how its action brought to life the way that human bodies move. It was very convenient, and believe it or not, once committed to memory it gave you the illusion that if you simply knew all the muscles involved in a movement, you would know everything there was about that movement.
The problem is you can't teach movement by diagramming the muscles.
Simply naming the muscles of the body, although convenient and sometimes impressive, does not really tell us how to deconstruct and reconstruct movement. History shows us that long before the muscles had been identified and named, people were moving in elegant and artistic ways to survive and seek independence throughout their lives.
The map of movement is obviously not the territory.
Next, my journey took me to physical therapy school, where instruction in finding impairments made the parts-based viewpoint even more convenient. Impairments is a word used to demonstrate the measurable deficiencies that we have in our human bodies, many of which revolve around stiffness and weakness, mobility problems and motor control problems, respectively.
If you take an orthopedic mindset, it's easy to see that maybe the underlying problem with your shoulder movement is your rotator cuff. That group of muscles isn’t really responsible for pulling, pressing and lifting things . . . what is does is hold your entire shoulder complex together.
.jpeg) Human joints (in this case, the shoulder) don't have a pin, or an axis holding them together. It's a ball and socket, with a few muscles pressing the ball and socket together, while the bunch of others simply try to pull them apart. It’s that “cooperation” that creates an axis of rotation, and therefore, movement. As I sat through some of my entry level orthopedic lectures, it became quite obvious that if somebody had shoulder disfunction, we could quickly do manual muscle tests and find weakness. Or, we could perform range of motion tests and find stiffness. With that knowledge gained, we could assign exercises to combat the weakness . . . or lengthening or strengthening exercises to combat the stiffness. If these situations were caused by an accident or an injury, then we might assume that prior to the accident and injury all things were normal; 100% of what we measured as an impairment was a result of the accident or the injury.
Human joints (in this case, the shoulder) don't have a pin, or an axis holding them together. It's a ball and socket, with a few muscles pressing the ball and socket together, while the bunch of others simply try to pull them apart. It’s that “cooperation” that creates an axis of rotation, and therefore, movement. As I sat through some of my entry level orthopedic lectures, it became quite obvious that if somebody had shoulder disfunction, we could quickly do manual muscle tests and find weakness. Or, we could perform range of motion tests and find stiffness. With that knowledge gained, we could assign exercises to combat the weakness . . . or lengthening or strengthening exercises to combat the stiffness. If these situations were caused by an accident or an injury, then we might assume that prior to the accident and injury all things were normal; 100% of what we measured as an impairment was a result of the accident or the injury.
That assumption is a pretty big guess. Basically, it says that people who simply seem to have orthopedic or movement issues, free of a neurological problem, have a neurological system that is at least optimized and is not the problem.
However, what if an accident or injury didn't occur and your shoulder became slowly dysfunctional over time. It seemed weak and/or painful and/or stiff. We would do many of the same tests, and say, "Well, you need to do strengthening exercises. And you need to do flexibility exercises." These might lead you to ask yourself, ‘You know, it's really funny. I don't do any more work with my right shoulder than my left. As a matter of fact, outside of handwriting and a few other things, my arms and shoulders have the same workload. They work off the same postural platform. They derive energy from the same neurological and metabolic system. And yet one is failing and yet one is flourishing. Are you sure I simply just need to exercise one side? Because they're getting the same exercise and one is breaking down, and one is thriving.’
How then do I reconcile this conflict?
Why am I assigning exercises to get somebody out of a situation, when a lack of exercise isn’t what put them in that situation?
The activity level of two shoulders was the same. How do I reconcile that? Do I simply assign exercises, and say you must do these for the rest of your life? Or do these simply jumpstart a system. And if they jumpstarted the system, what caused the problem in the first place? Two shoulders with the exact same work and activity load, one gets worse, one gets better. Why?
Did you catch yourself looking for a bad part? We always want to find a bad structure.
Maybe we simply have bad behaviors . . . and find dysfunction.
In my brain, I had assumed that function was governed by structure. I never pondered the reverse relationship.
I didn't really know how to reconcile that shift in focus until I started taking classes that discussed the neurological explanation of movement in PT school. I was introduced to two concepts: The postures and patterns we go through in the developmental sequence early in life, where babies explore rolling, creeping and crawling in the transitions up to standing. Then follows stepping, balance, gait and eventually running.
These postures and patterns occur spontaneously in growth and development if a child is well rested, well fed and in a safe environment. They simply explore postures and patterns the exact same way they grow their bones and develop their muscles. They are simply driven to do so and, if not interfered with, they will do it in a very systematic and elegant way.
PNF (Proprioceptive Neuromuscular Facilitation)
We learned how to use postures and patterns to jumpstart the neurological system. These aren’t focused on the impairments or a specific body part, but instead concentrate on the synergy and complimentary aspect of body parts working together.
Babies are born with too many physical impairments to walk. They resolve them by doing what they can in a more functional manner . . . and the impairments go away.
The shoulder does not work independently. It works with the shoulder girdle, and the shoulder girdle anchors itself on the spine. Many of the things we do with the shoulder aren't directed by an intention of the shoulder. They are directed by an intention of the hand; The way you use your hand influences the way you use your shoulder. Likewise, the way you hold your spine influences the way you use your shoulder. The pattern that you want to accomplish and the posture that you choose take you there are both ends of what's going on at the shoulder. In most cases, the shoulder is basically listening to the commands of the hand and responding to the integrity of the posture. It was a far cry from simply going through the body and simply measuring impairments.
There are two ways to exercise a weak rotator cuff. One way is to find out if somebody is weak in external rotation. And we can measure that in certain positions just by having you create a force into external rotation. I think we can all imagine what that test looks like. It's a very sterile test that has us work our shoulder in one direction. One of the central mistakes we make there is to assume that practicing the test will fix the impairment; “Well if we're weak in that direction, let's just cut off a piece of rubber band, and you can repeat that motion until the day you can come back in, and we can re-test your rotator cuff.”
The other way to strengthen the rotator cuff is to do the exact same impairment test we were taught to do in orthopedics with external rotation, but also explore the PNF patterns. These are called Diagonal One, and Diagonal Two patterns and cover both flexion and extension. In exploring these four patterns, you simply use the array of muscles in a spiral and diagonal way to complement each other, using them in unison. Many of the natural activities we do, throwing, striking, lifting, pulling and pushing are simply slight deviations from the flexion, extension, D1 and D2 patterns of the upper body. And yes, these patterns exist in the lower body too.

.jpg)
My first conflict: Even if I could measure rotator cuff weakness in an isolated test, do I simply strengthen the rotator cuff using exercises that resemble the test? Or, do I throw that shoulder into a more complex natural pattern, knowing very well that if the rotator cuff is the weakest link of this pattern, then it will obviously receive the most benefit? While it's getting stronger, it's also learning how to interact in synergy. Through timing and coordination, it’s complimenting the other muscles above and below it, working with them and in opposition.

In short, my orthopedic background was telling me to isolate, identify parts, measure impairments and relate those back to function and movement. My neurological exposure was telling me to look at postures and patterns and realize that the whole is always greater than the sum of its parts.
Orthopedics seemed clean, clear and concise. Neurological seemed messy, broad and complex . . . but it also seemed to have a better overall perspective when you backed away from movement.
Before I could resolve this, I developed another conflict. After physical therapy school, I started studying manual therapy as deeply as I could. Manual therapy showed me a way to take a head-to-toe approach to orthopedic therapy, and really consider all the moving parts. With a much more thorough diagnosis, came the realization that, often, there’s not just one problem. There are multiple problems, usually with a catalyst.
A single dysfunctional movement forces multiple impairments to be confronted as a whole instead of in isolation. That doesn’t discount in any way the contribution of impairments measured in isolation . It’s not a solution, just a parallel gauge of different perception.
It was also through my manual therapy exposure that I learned the problem isn't necessarily where the pain is.
Long before we had the term regional interdependence, I was realizing that body parts that were behaving poorly (bad function,) but not having pain, could actually be a greater problem than a body part that was having pain but well-behaved (good function.)
Still, the fact that we saw pain in one area blinded us to the dysfunction that was supporting the situation in the first place. We call it compensation. One body part has to work overtime to make up for another that's not behaving well. The one not behaving well is actually the problem, even though it may not be the pain.
I delved into more thorough movement examinations. I got a lot of perspective and ideas from the in-depth way that manual therapy achieves an orthopedic diagnosis, compared to the convenient way that kinesiology and biomechanics inform an orthopedic hypothesis. While it’s convenient to identify a faulty part and train that part in isolation (or simply get an orthopedist to replace that part), that path rarely restores the whole to anything that resembles its original function. It's a band-aid, or a brace at best.
We still need our impairment measures because they help us realize the local changes we're making. But we also need a perspective that keeps us from practicing a test, so we can see true change, as opposed to synthetic change that is simply propped up by temporary activities that will soon be gone, to be followed by the positive change itself.
If I:
1. Use a head-to-toe manual therapy perspective to not only identify dysfunctional body parts, but painful body parts as well, and . . .
2. Use a neurological integration model as my rehabilitation vehicle . . .
3. Then maybe I can reconcile the fact that orthopedics demands we look at parts and measure impairments.
There is nothing wrong with that and we should do it. But, if we can’t reconcile those steps with the movement behaviors, then we will not be dispensing complete rehabilitation when something happens in your movement life.
There is nothing wrong with measuring impairments. What is wrong is trying to fix them the same way that they were measured. That leaves you practicing the test with isolation exercises, not integration exercises. It leaves you assuming that, if the impairments have been managed, then movement will spontaneously restore itself.
Good movement keeps impairment at bay.
My realization took the opposite route: We should focus on movement and take you to the point where you still have movement competency to find that edge where your movement competency starts to erode and where you start making compensations and mistakes. Once we’re there, we have you reconcile those behaviors at that level. Not only will your impairments start to resolve themselves, but you will be resolving those impairments without practicing the tests that identified them. That means you have a truly organic remedy to a synthetic test measurement.
If we truly believe that the whole is greater than the sum of its parts, then we realize that simply making the parts better may not get us the whole. In our case, that whole is complexity of movement. We need a movement evaluation tool right alongside our impairment and parts evaluation tools. We must work to reconcile the movement information with the impairment information whenever possible. We must also remember that the pain may not be where the problem is and the problem may not be where the pain is.
1. Map problems like an orthopedic expert.
2. Treat through postures and patterns, following a neurological progression.
3. Whenever possible, use orthopedic methods to improve sensation while providing sensory-rich opportunities to perceive and process the new information.
Measure global movement and local input. Reconcile what you find.
Click here for the next installment of the Conflicted series.
Posted by Gray Cook
Posted by FMS
This is one of the most valuable articles I have ever read when it comes to looking at and evaluating movement. Thank you Gray.